Introduction
I call melatonin the miracle molecule, because it protects us and improves our health, vitality and lifespan. Melatonin is best known for the part it plays on our circadian rhythm, stimulating us to sleep at night. Many healthcare practitioners are not fully educated on how safe and effective melatonin can be. Taking melatonin in doses up to 60 or 300 mg, or even 2 mg, can help with a variety of conditions. Additionally, dosing melatonin both night and day, with various protocols, has been gaining vast popularity in alternative medicine. It is all deeply based in a wide body of research, which has proven melatonin to be one of the most protective and necessary molecules our body produces. In this article, we will take a deep dive into autoimmune conditions, and consider recent discoveries as well as ongoing research about melatonin effects on these conditions.
What is Melatonin: Background on the miracle molecule.
Melatonin, known as N-acetyl-5-methoxytryptamine, is the main secretory hormone produced by the pineal gland during the night. It regulates the circadian rhythm and seasonal changes in vertebrate.[1] It is the main hormone produced when we are going to sleep and helps us to stay asleep. It was first discovered by McCord and Allen in 1917, when they found that a substance extracted from the bovine pineal gland whitens the skin of Rana pipiens, and they name it melatonin.[2]
Autoimmune diseases are conditions in which the body’s immune system mistakenly attacks healthy cells, tissues or organs, and mouse an attack through your immune system against them. This results in different disease conditions such as type 1 diabetes mellitus, ALS, systemic lupus erythematosus, multiple sclerosis, inflammatory bowel disease, and rheumatoid arthritis.
Biological Effects of Melatonin
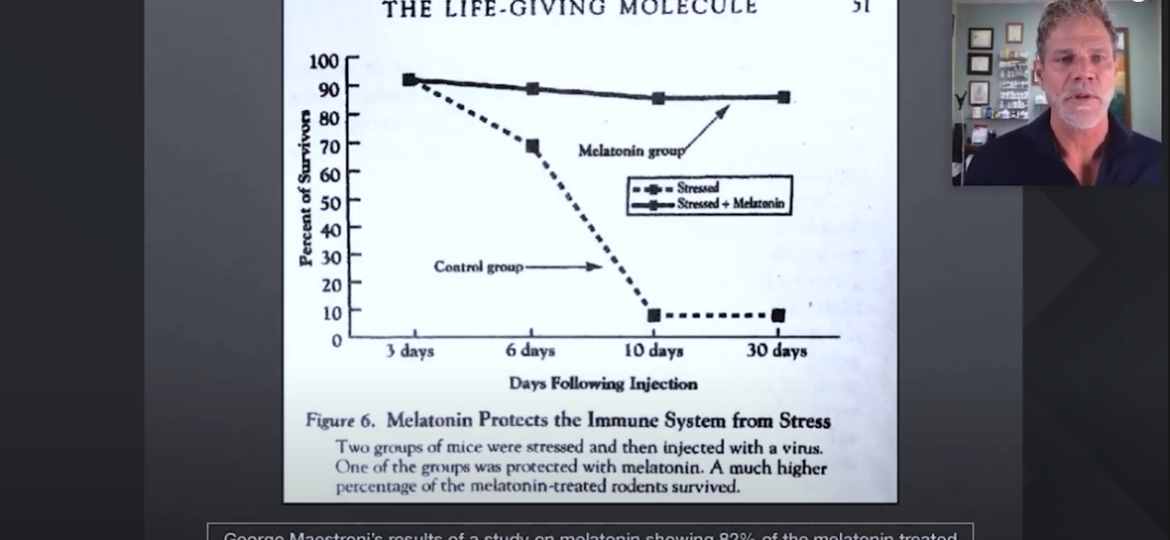
Melatonin is considered a pleiotropic molecule, with both pro-inflammatory and anti-inflammatory properties. It is immunomodulatory, meaning that it reduces excessive immune function in inflammatory conditions, while improving immune conditions in immunocompromised individuals. So you could say melatonin is truly adaptogenic, meaning that it is ready to meet whatever needs it calls for.
Melatonin receptors are seen in a wide variety of immune cells.[3] This means melatonin has an influence on almost your entire immune system! Cells like CD4+ T cells, CD8+ T cells, and B cells,[4] are cells that are used to kill invading pathogens, as well as help you to produce antibodies to protect you from future infections. I’m going to get a little bit deep here with studies, so if this isn’t your interest skip to the next section.
Here is a study showing that treatment with melatonin enhances the production of natural killer cells and monocytes in the bone marrow of mice.[5] Other studies also show that mice treated with melatonin have decreased expression of interleukin (IL)-2 and interferon (IFN) gamma. At the same time, there is an increase in the production of T helper cell cytokines like IL-4 and IL-10.
Melatonin is also essential in the development of T helper cells. The balance of T helper cells is crucial in regulating cellular immune responses.
T helper 1 (Th1) is important for inflammatory responses by producing pro-inflammatory cytokines such as IFN-y and IL-2.
However, T helper 2 (Th2) is anti-inflammatory and produces cytokines such as IL-4, IL-5, IL-10, and IL-13.[3]
Studies show that low doses of melatonin increase Th1 cytokines, thereby increasing inflammation, while high doses of melatonin reduce pro-inflammation, thereby reducing inflammation.
Melatonin and Autoimmune Diseases
Autoimmune diseases could be classified as either organ-specific, such as found in type 1 diabetes mellitus, or systemic as in systemic lupus erythematosus. Where in the United States, autoimmune diseases are said to affect about 5% of the population.[2] This results from the activation of immune cells and T and B cells discussed earlier, by antigens on the body tissues, which the body mistakenly sees as a threat. Activation of these immune cells by this antigen results in damage to target tissues by the activated cells. This is where I need to interject my personal opinion: autoimmune conditions don’t just happen for no reason. Some of the factors at the root of this is chronic toxicity, chronic infections and imbalances in the digestive track leading to either dybiosis or leaky gut syndrome. All of these cause inflammation, which regulates cytokines. They then break down your cells ability to make energy, which results in the ability to have a proper regulated immune system. Besides having an improperly regulated immune system, there are also specific triggers to the immune system, whereby the immune system gets confused and the information is encoded in order to attack a specific tissue in the body. Toxins can settle in certain areas and tissues of the body, and infections can enter inside of cells. The immune system is trying to get that intracellular infection. Chronic activation of the immune system through gut issues, constantly triggers the immune system which eventually switches and starts attacking your own body. Although we are diving into melatonin in this article, these considerations need to be addressed along with melatonin supplementation, in my opinion. Without addressing the root cause, it will be like bailing a leaking boat or painting over rust. You can reference ultimatecellularreset.com for more up-to-date information about melatonin as well as other strategies for autoimmune conditions.
So, melatonin is an immunomodulatory hormone, which has been shown to have a regulatory impact on the pathophysiology of these diseased conditions. Understanding this mechanism can help in the use of melatonin supplements in alleviating symptoms and slowing the progress of the disease.
We’re going to take a look at a variety of different auto immune conditions and consider the latest research using melatonin and how it might affect the specific conditions. Conditions such as Type 1 Diabetes mellitus, Multiple sclerosis, Systemic lupus erythematosus, inflammatory bowel diseases, and Rheumatoid arthritis.
Pathophysiology of Type 1 Diabetes Mellitus
Type 1 diabetes mellitus (T1D) is also known as insulin-dependent diabetes mellitus. This autoimmune disease results from the destruction of beta cells in the pancreatic islets, which is responsible for producing insulin. It is also called childhood or juvenile-onset diabetes, because it usually starts at childhood with symptoms of polydipsia (increased thirst), polyphagia (increased eating), and polyuria (increased urination) with associated weight loss.
This autoimmune disease is T cell-mediated.[6] There is hyperglycemia, ketosis, insulitis, and the presence of anti-islet antibodies, including anti-glutamic acid decarboxylase (GAD) antibodies, anti-insulin antibodies (AIA), and IA-2 autoantibodies.
Melatonin Modulation of Type 1 Diabetes Mellitus
In type 1 Diabetes mellitus, the destruction of insulin-producing beta cells results from the activation of pro-inflammatory cytokines such as TNF-alpha and IFN-gamma, which are mediated by Th1 cells.
Studies carried out on non-obese diabetic mice, an animal model of T1D, show that prolonged administration of melatonin resulted in increased survival and delayed onset of diabetes.[7] Melatonin helps shift the immune response from Th1 cells to Th2 cells, thereby reducing TNF alpha and IFN gamma production, which protects against beta-cell destruction.
Studies also show that pancreatic islet grafts done for diabetic mice increased survival rate from 7 days to 17 days when melatonin was administered.[8] This pancreatic islet graft is a potential surgical therapy for T1D by administering melatonin to prevent the graft from attack or rejection.[9]
Pathophysiology of Multiple Sclerosis
Multiple sclerosis is a chronic inflammatory demyelinating disease of the central nervous system. It results from the loss of the neuronal myelin sheath due to attack by autoantigen-specific immune cells. This leads to pain, fatigue, body weakness, and even vision loss at times. The onset of the disease is usually between the age of 20 and 40 years.[10]
The pathogenesis of multiple sclerosis involves both the adaptive and innate immune cells. Experimental autoimmune encephalomyelitis (EAE) is the commonly used animal model for multiple sclerosis due to its close similarities.
Findings show that animals with EAE have T cells and macrophages infiltrating the CNS lesions. This autoimmune process is initiated by the adaptive immune CD4 T cells, which results in the production of inflammatory cytokines by the innate immune cells like macrophages. These pro-inflammatory cytokines result in severe inflammation and damage to the myelin sheath and neurons seen in EAE.[11] The production of reactive oxygen species in the affected areas as markers of oxidative stress is increased in the neurons of Multiple sclerosis patients.[12]
Melatonin Modulation of Multiple Sclerosis
Findings show that there is dysregulation of melatonin production in patients with multiple sclerosis. There is an excretion of a high amount of melatonin metabolites in such individuals urine at night.[9] This means that such patients have a reduced level of melatonin, this is correlated to the fluctuation of multiple sclerosis symptoms.
In multiple sclerosis, there is the activation of Th17 cells, which worsens the inflammation. Melatonin suppresses the Th17 cells, which helps slows down or stop the progression of the disease.[13]
Pathophysiology of Systemic Lupus Erythematosus
The systemic lupus erythematosus (SLE) is an autoimmune disease characterized by malar (butterfly) rash, photosensitivity, nephritis, and arthritis.[14] It results from damage to tissues by immune cells. SLE affects more women than men, and can manifest at any age.
In SLE, there is an activation of autoreactive T cells, resulting in B cell hyperactivity. This leads to the production of Th1 cytokines such as IL-2 and IFN-gamma as well as TH2 cytokines IL-4. SLE also shows increased levels of inflammatory cytokines TNF-alpha and IL-6.[15]
Melatonin modulation of Systemic Lupus Erythematosus
Researches show that melatonin administration can be helpful in the treatment of SLE. The mice model of SLE shows improvement for symptoms after the administration of melatonin. However, the effects of melatonin administration are time-dependent as well as gender-sensitive.[16]
When melatonin is administered to female mice in the morning, there is an increase in survival rate, and symptoms improve. However, when administered in the evening, there is no noticeable improvement.[17]
For male mice, however, the effect of melatonin is different. Melatonin treatment of SLE in male mice worsens the symptoms by increasing inflammatory cytokines and autoantibodies. This effect in males may be due to testosterone, which increases pro-inflammatory cytokines when combined with melatonin.[18]
Therefore, for patients with SLE, melatonin supplements will benefit female patients and should be used in the morning.
ALS and Melatonin
In ALS, oxidative stress is a common molecular denominator of the disease progression. Melatonin shows that it processes a unique spectrum of antioxidative effects, not conveyed by classical antioxidants. Do you to this unique antioxidant property it shows effectiveness against ALS in super physiological doses. In a study performed in 2006 called, “Reduced oxidative damage in ALS by high-dose enteral melatonin treatment”, they used 300 mg melatonin suppositories once a day. This is a section reported in the study.
“In a clinical safety study, chronic high-dose (300 mg/day) rectal melatonin was well tolerated during an observation period of up to 2 yr. Importantly, circulating serum protein carbonyls, which provide a surrogate marker for oxidative stress, were elevated in ALS patients, but were normalized to control values by melatonin treatment. This combination of preclinical effectiveness and proven safety in humans suggests that high-dose melatonin is suitable for clinical trials aimed at neuroprotection through antioxidation in ALS.” [18]
I suspect the results would be better in many of the studies where the dosing was performed poorly, than if the study was done using suppository form. Studies show that oral absorption of melatonin is only 2.5% absorbed [19], whereas a suppository bypassing the gut and digestive enzymes as well as first pass through the liver, would have a much higher absorption.
Conclusion
In conclusion, anyone with an autoimmune conditions should seriously consider Element in with a quality melatonin. The question is how much melatonin should one use? Will I shut down my normal production of melatonin and if I take high doses of melatonin? Is that dangerous? Anyone that is looking to deal with sleep issues, as long as they’re not trying to reset their circadian rhythm in a separate time zone, will be fine with doses of melatonin from 3 to 20 mg. There’s something called super physiological dosing of melatonin where doses up above 40 all the way up to 200- 300 mg are taken. These doses are both safe, as studies show that even up to 150,000 mg of melatonin would not cause any toxicity. [20] In addition to that unlike most hormones, melatonin does not create a negative feedback on your brains production of melatonin. Anyone suffering from an autoimmune condition, may consider taking higher doses of melatonin. Due to melatonin only being 2 1/2% absorbed orally, [19] some may consider the use of a suppositories or even a liposomal delivery such as with Sandman. In addition to melatonin supplementation, it is advised to seek the care of a functional and or naturopathic practitioner who can run the right laboratory tests, to determine what is at the root cause of the autoimmune condition. Once they have this knowledge, they can work on correcting the underlying problem while continue your melatonin protocol. For more information about melatonin and advanced naturopathic strategies go to ultimatecellularreset.com or you can read my book Melatonin: The amazing benefits of the miracle molecule. available on Amazon in 2021.
John Lieurance, ND, DC, DABCN (board eligible)
Dr. John Lieurance is a speaker, author, healthcare educator and scientist. He is currently in private practice since 1996 as both a Naturopath and Chiropractic Neurologist. He is the chief scientific officer of MitoZen Scientific who makes cutting edge natural healthcare technologies. He is also the director of Advanced Rejuvenation in Sarasota, Florida, a  regenerative practice focusing on chronic disease and regenerative medicine. You can follow Dr. Lieurance and his online education at ultimatecellularresort.com. Dr. Lieurance is available for distance consultations and for patients to travel to his clinic in Florida for personal care. Dr. Lieurance’s focus includes traumatic brain injuries, vestibular disorders, degenerative neurologic disorders, inner ear regeneration, autoimmune conditions, mold illness, Lyme disease, chronic viral infections, detoxification protocols and orthopedic ultrasound guided regenerative medicine using stem cells and platelet rich plasma.
regenerative practice focusing on chronic disease and regenerative medicine. You can follow Dr. Lieurance and his online education at ultimatecellularresort.com. Dr. Lieurance is available for distance consultations and for patients to travel to his clinic in Florida for personal care. Dr. Lieurance’s focus includes traumatic brain injuries, vestibular disorders, degenerative neurologic disorders, inner ear regeneration, autoimmune conditions, mold illness, Lyme disease, chronic viral infections, detoxification protocols and orthopedic ultrasound guided regenerative medicine using stem cells and platelet rich plasma.
This article is for informational purposes only . It is not considered to be medical advice and anyone looking to start any melatonin protocol, should do it with the advice of their healthcare practitioner.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b1-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#:~:text=Melatonin%20therapy%20has%20been%20investigated,rheumatoid%20arthritis%20and%20ulcerative%20colitis.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3645767/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b17-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b20-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b100-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pubmed/8797184/
- https://www.ncbi.nlm.nih.gov/pubmed/19708865/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b64-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b67-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b70-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pubmed/27561251
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b78-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709754/#b79-ijms-14-11742
- https://www.ncbi.nlm.nih.gov/pubmed/22288898/
- https://www.ncbi.nlm.nih.gov/pubmed/8586486/
- https://pubmed.ncbi.nlm.nih.gov/17014688/
- https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-079X.1997.tb00302.x
- https://onlinelibrary.wiley.com/doi/abs/10.1211/002235702760345374